The World is just recovering from the wrath of the deadly Covid 19 and India is slowly healing itself from the clutches of a devastating second wave with an unprecedented toll in April and May 2021. While the crisis is still not over with fate of 100 crore Indians still looming at large largely from the uncertainty of future – if there will be a third wave, if there will be vaccines available on time, if the economy will be up and running etc
I have been pondering for long and have finally decided to write about my own experience battling Covid as a patient and treating Covid patients as a doctor for the past 16 months since March 2020.
The First Wave
It all started as a distant affair – news of loads of patients testing positive and numerous people dying from lack of hospital beds and ICU support. It all began for me in March 2020 when it was making news in the West – Italy followed by other European countries and simultaneously in the US.
The Indian Government was quick to act, taking lead from the happenings from other part of the World. Lockdown was imposed by third week of March 2020. The total number of Covid cases around third week of March 2020 was few thousands (3000 – 5000) at that time – nothing compared to the astronomical numbers seen in the second wave ( more than 4 lakh new patients testing positive in a day in May 2021).
The next two months were relatively slow. Not many Covid patients – still learning about the treatment protocols from the western countries, US and Europe and their experience. The total numbers were gradually increasing but not to the extent unmanageable till end of June 2020 when hospitals started overflowing.
By mid July, Covid spread its tentacles far and wide in the Country and every state was reporting record numbers – mainly Maharashtra, Kerala, Tamil Nadu and the northern states of Delhi etc. My hospital saw beds getting filled up to the extent – our regular ICUs were filled and a makeshift ICU for non covid patients had to be opened in a separate floor.
My First Covid experience as a patient
I tested positive in early July 2020 after few of the operating room staff tested positive and I had mild symptoms and got myself checked and it turned out me and my perfusionist both tested positive.
Fortunately, CT scan was normal and inflammatory markers like CRP, Ferritin, LDH were also normal. Over the next couple of weeks, it was a game of isolation and quarantine and waiting for the body to clear the virus. While there weren’t lot of symptoms, I still had tachycardia with very minimal exertion like climbing two flights of stairs – things which weren’t the norm before. Earlier, I used to regularly work out in the gym and do Cardio for 20 – 30 min daily, 4-5 days a week.
After about two weeks after testing positive, I became negative to the relief of my family and everyone. I was relieved. I started attending to my regular hospital work. This time Covid was at it’s peak in India. It was August and September of 2020 and the scenario everywhere was overflowing beds – ICUs were full and beds and ventilators weren’t available. There were regular news of near and dear ones dying etc.
I had gotten my hands full in managing Covid patients. I had the opportunity of initiating ECMO in few of the critically ill Covid patients. I was keen on trying to help the Covid patients out of sense of responsibility and of the unfound belief that I had gotten infected with Covid once and recovered and hence I am relatively immune to Covid.
My Second infection with Covid
Little did I know that I had gotten lucky the first time (probably because of infection with a lower viral load) but neither was I a superhero nor my body was super immune nor had any extra resistance to ward of a second infection.
I was called in to initiate ECMO for a critically ill Covid patient who happened to be a close relation of the Chief Minister of a neighboring state. The patient was critically ill with near total lung involvement and poor oxygenation and impending failure of other organs as well. ECMO was initiated as per usual protocol and everything was fine till about next day when I started having fever and bodyaches.
I brushed it off as fatigue and regular ill feeling after a night up. However, the low grade fever persisted two more days and by then I could know that I had lost my sense of smell and food was tasteless. I knew that I had gotten infected with Covid a second time. I had given an RT -PCR swab and it indeed was positive as I had expected. Since my saturations were normal and did not have any breathlessness and screening CT showed about 10% lung involvement (few ground glass opacities in the right lower and left upper lobe) I was hoping that this time too it will be a passing phenomenon.
I was on the usual medications – vitamin C, Zinc, antibiotics and Inj Remdesivir. I had isolated myself for 2- 3 days. It was already 6th day of illness when I got checked and CT scan was done and started on Inj. Remdesivir. I used to visit the Covid section in the Emergency for my injection and then come back home to be in quarantine.
However, on 9th day, after my dose of Inj Remdesivir which I had received in the ER, I had developed severe chills with rigors. It settled after the usual cocktail of antihistamines etc
Over the next two hours, I couldn’t gather myself up and my plight worsened. I was semiconscious and I was not aware of what was happening around me. As I was in isolation upstairs at my home, I couldn’t call anyone for help. I was not aware when I had become unconscious and fallen down. My wife (who was downstairs) heard a loud thud and knew something was wrong and then tried to reach me on my phone. She had to rush and check out herself as there was no answer. By then, I could gather strength to wake up and realize what was going on and told her that it’s time for me to get to the hospital and get admitted.
As the ambulance had a lag time, my wife decided to drive me to the hospital after I managed to walk to our front door. I once looked back at my house and thought if I will ever get back home, if I will ever get to see my kids again. Both of my kids were sleeping and were oblivious of what was happening.
Once I came to the ER, it was a different perspective being a patient as against being a doctor who is used to treating the patient all my life. I felt helpless, weak and tired. My blood pressures were low (systolics in the 80s ) and dehydrated. I still couldn’t move much or get out of my bed. Fortunately I knew most of the people there as it was the same hospital where I worked and everyone were my colleagues. All my lab parameters were deranged.
I was shifted to the ICU for monitoring. Over the next 24 hours several investigations were done and it was a shock to many of my colleagues. Until then, it was business as usual treating Covid patients and people were living with a sense of false security that they were immune. I was the second one in the hospital to become positive a second time (after one of my ER colleague who became positive a second time and was having hell of a time) and it was well evident now that Covid can cause reinfection despite previous infection (against popular perception and evidence).
My inflammatory markers were all elevated – CRP, Ferritin, LDH. Interleukin levels were elevated. The procalcitonin was through the roof. Our pulmonologist suspected cytokine storm and promptly initiated treatment. The puzzling thing at that time was minimal lung involvement and saturations maintaining but with lab parameters abnormal and indicative of cytokine strom.
Today, we now know that Covid can cause Multisystem Inflammatory Syndrome (called MIS) as it is called which is a predominant form of vascular inflammation without much lung involvement. During the first wave, it was more of learning and there wasn’t much literature on MIS.
However, our hospital Pulmonologist took the lead and she put in all knowledge and experience she had gathered over many months treating hundreds and thousands of Covid cases. I was on pulse steroids, highest antibiotic cover and the whole cocktail of medicines – antiinflammatory, oral hypoglycemics, blood thinners etc
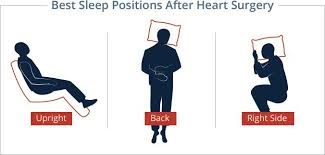
I was in the ICU for 3 days and in the ward for another three days and finally was discharged after a week once my lab parameters started trending down. They had not normalized completely. I was feeling weak, tired, occasionally breathless if I exerted. I had lost some weight. But I was grateful to be alive and to be back home and see my family and kids.
There was still a lingering sense of unease about anything bad that might happen. I had seen my share of complications ranging from stroke to heart attack to sudden death from large pulmonary embolism in patients with recent Covid. There were patients who had come with sudden loss of blood supply to their arms and legs and even losing limbs.
However, I had made an uneventful recovery by the grace of the almighty. After about two to three weeks rest, I was finally ready to be back to my usual domain where I have spent most of my life – operating room and ICU.
By that time, Covid had started waning in many parts of the country and people were thronging the streets and there were very minimal precautions if any followed by the public. Many were still using masks, however, the social distancing and sanitizing norms were forgotten. News of vaccines waiting for approval were like music to the ears. Around this time (November and December 2020) the US was badly hit by the second wave with daily new cases averaging 2.5 lakhs and large number of deaths (around 4000 – 5000/day)
World media were praising India and the people and the administration as to how India had won over Covid while the rest of the world was struggling. In retrospect :- It was a word spoken too early.
While the next couple of months (Jan and Feb 2021) were okay – with life returning to normalcy relatively and large number of heathcare and frontline workers receiving the vaccine shots. Many were of the conclusion that Covid was over.
The Second Wave
By third week of February there was news trickling in about new cases of Covid being reported in multiple states – mainly Maharashtra and New Delhi and in other parts of the country as well. Over the next 2 – 3 weeks, it was like Deja Vu with things playing back again like last year.
By end of March 2021 and early April, hospital where I worked started seeing increasing admissions and sicker patients. This time, it was a large proportion of younger patients in their 30s and 40s compared to the first wave. By end of April and early May, it was complete mayhem and chaos. People were asking for hospital beds to be reserved, news of known people and relatives dying an untimely death were regular almost every other day. It was all the same again – play back of last year with uncertainty, impending doom, mood disturbances and dismay at seeing suffering and agony everywhere. Videos and news feeds of burial grounds showing tons of people being cremated – caused psychological disturbances and was emotionally draining. There were several nights where I woke up for no reason with a sense of unease and had difficulty going back to sleep. I just prayed to God and wondered if God is indeed there, that he take stock of the situation and guide humanity and mankind.
Today, even as I write this in June 2021, there is doubt of impending third wave as lockdown restrictions have been lifted. There is still so much uncertainty and more questions than answers which only time can answer.
#surgeonwithcovid
#frontlineworkers
#doctorscovid
#Covid_19SA / #Coronavirus / #Covid19
#StaySafeStayHome
#staysafe #stayhome #StaySafeStayHome
#WFH
#WorkingFromHome #Lockdown
#covidiots
#FlattenTheCurve